HIV Tongue: [See Pictures] identify Symptoms at every HIV stage
HIV tongue signs occur mainly during its oral manifestation stage. The signs on the tongue indicates compromised immunity.
These signs appears usually during the secondary stage of infection, when the patients with HIV are susceptible to many types of infections (due to compromised immunity). This usually happens when there is a drop in the CD4+T count.
There are many of conditions appearing on the tongue (leukoplakia, candidiasis & ) indicating that who might have HIV virus in your body.
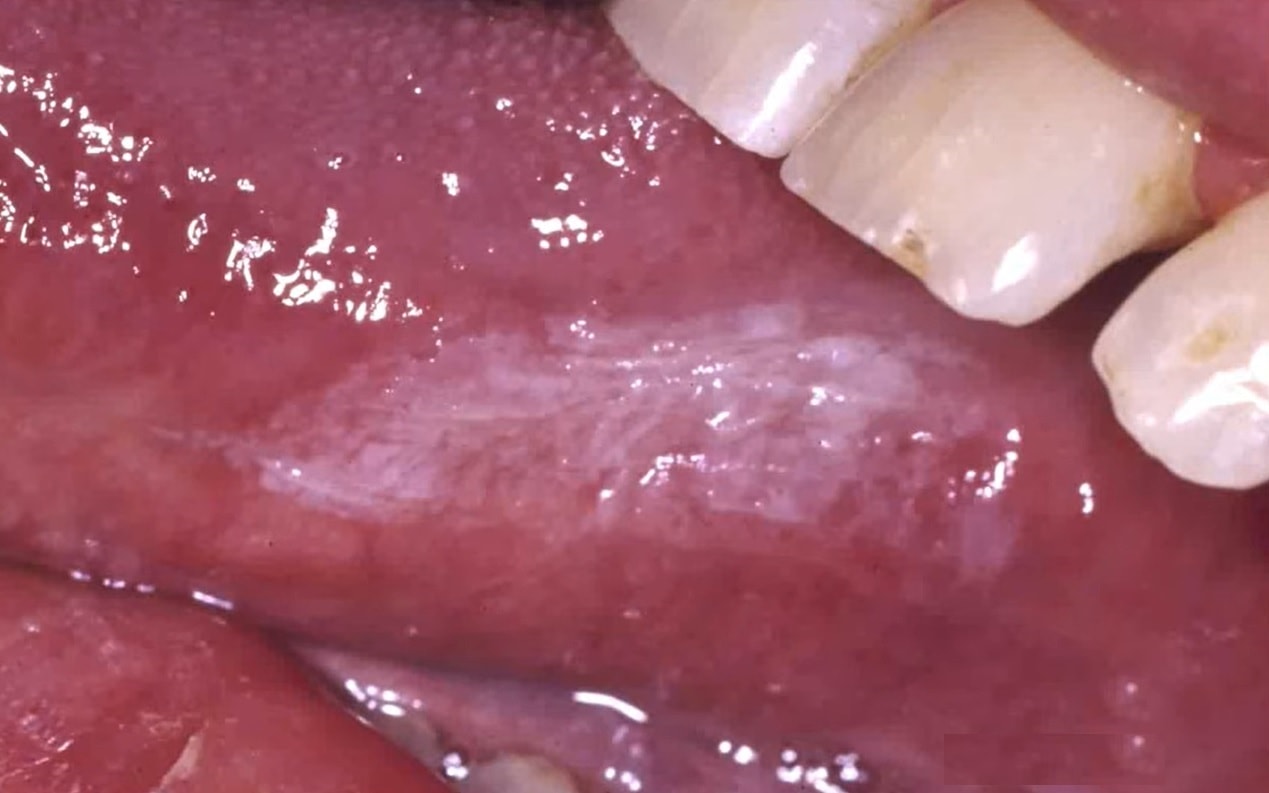
Oral Hairy Leukoplakia
It’s a white lesion that shows up on the lateral border of the tongue it does not wipe away. As the characteristics distribution is on the sides of the tongue and with the linear striations.
If the patient has these kinds of oral lesions suggesting oral hairy leukoplakia this does indicate some level of Immunosuppression, particularly category B classification, indicating moderate immune suppressions. This is one of the common symptoms which occurs during the initial stage of HIV.
One condition for Oral Hairy Leukoplakia is you are not going to see this lesion in a person who has an undetectable viral load. So if you were working in an urgent care setting and you saw somebody present with shortness of breath and you had a chest x-ray with diffuse infiltrates you look in their mouth and saw this putting two and two together you could conclude there’s a significant likelihood this person has HIV infection.
Besides HIV, these lesions condition can also be seen in rare cases of transplantation or other severe immunocompromised patients.
Treatment
These lesions tend to go away after antiretroviral therapy for about three to six months but of less effect. You can use a high dose of antiretroviral regimen, acyclovir it will lessen the symptoms but the lesion will come back.
Also Read: What does HIV rash looks like?
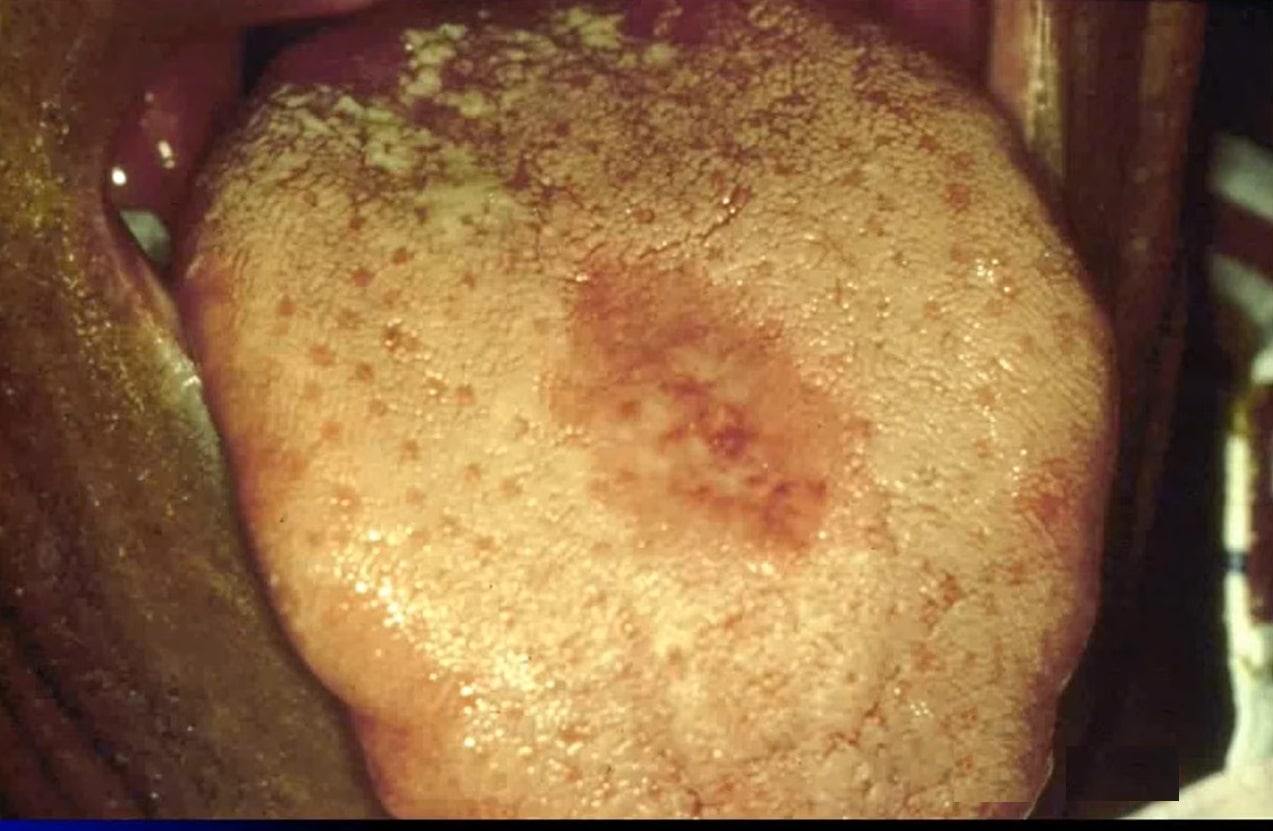
Oral Erythematous candidiasis
It is probably the most overlooked lesion that we see in association with HIV. It presents as a red flat subtle lesion either on the dorsal surface of the tongue and/or the hard palate.
On the tongue it can also have a red slick spot that you can also see on the roof (palette). Another symptom is the burning sensation, lack of taste also accompanies candidiasis.
Patients will complain that their mouth burns or their tongue burns especially when having salty or spicy foods or acidic beverages such as orange juice or grapefruit juice.
This is a kissing lesion so if you see a lesion on the dorsal surface of the tongue, take a look up at the hard palate and see if you see a matching lesion.
Treatment
In the above case there are other things that this might look like Pizza burn, but unlike a pizza burn which go by its own, oral erythematous candidiasis requires therapy and topical therapy is recommended to treat erythematous candidiasis in some cases systemic antifungal therapy is also used. This treatment should last 2 weeks to reduce the colony forming as much as possible.
Also read: Can you get HIV from swallowing semen (cum)?
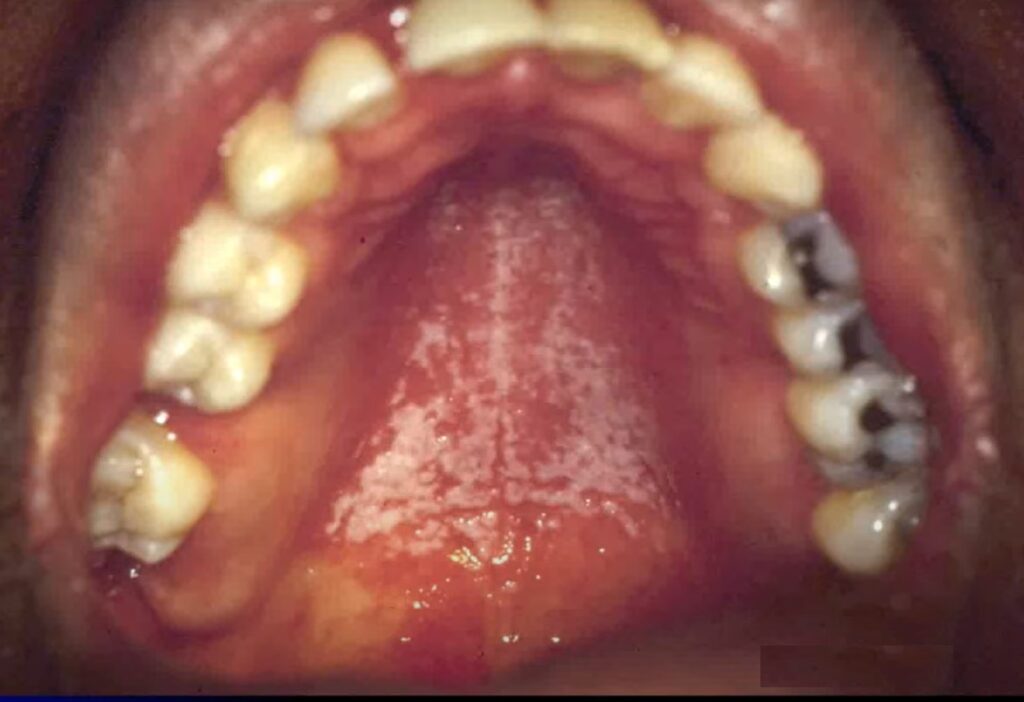
Oral Pseudomembranous Candidiasis
This type is the one most commonly found candidiasis which is associated with HIV, the pseudomembranous candidiasis or the common term you her people use for this is ‘thrush’.
It affects mostly on the tongue and on the palette region.
The phases of the disease has been divided into two based on the treatment
- Mild to Moderate Pseudomembranous Candidiasis
- Moderate to severe Pseudomembranous Candidiasis
a) Therapy for Mild to Moderate Pseudomembranous Candidiasis
For mild to moderate oral candidiasis can be treated using Topical agents such as Clotrimazole troches and Nystatin oral suspension.
Topical antifungal therapies work by coming into contact with the candida plaques and disrupting cell function.
So topicals actually have to be able to get in touch with the lesion so if it’s further back in the posterior oropharynx it may not work & at that point you may require Systemic therapy.
Use coupon code=10OffOrder or click here to get $10 off on your HIV test
b) Therapy for Moderate to severe Pseudomembranous Candidiasis

So, where the plaques is present the medication may not come in contact with the lesion. As the topical therapies involves gargling. The medication just couldn’t establish the with the plaques and the posterior oropharynx on the uvula long enough to actually and have the desired effect.
Here, we use systemic therapies and there are two listed the most common and by far the most used is Fluconazole & Voriconazole which is take two on the first day and then one for the rest of that two-week period of time
Note: Topical antifungal therapies work by coming into contact with the candida plaques and disrupting cell function so topicals actually have to be able to get in touch with touch with the lesion so if if it’s further back in the posterior oropharynx.
Angular Cheilitis

The third major type of candidiasis associated with HIV that you see is what’s called angular cheilitis.
It presents as a cracking or fissuring at the corners of the mouth.
Also, people may just describe sort of a burning or chafing on the corners of their mouth
Treatment
You can manage the angular cheilitis with ‘topical therapy’ as long as they don’t have any significant intro oral candidiasis
Aphthous Stomatitis
Above is the case of Aphthous Stomatitis or Aphthous ulcers which was brought up in differential diagnosis. The above is a severe case of Aphthous Stomatitis with severe symptoms and multiple aphthous ulcers appearing in different areas of the mouth (tongue, roof of the mouth, in the buccal mucosa and causing pain and discomfort.
Severe Aphthous Stomatitis or in its advanced stage may find it difficult to respond to topical anesthetics, or topical corticosteroids, and with subsequent multiple episodes it can lead to repeat courses of oral prednisone.
Thalidomide is the effective therapy in treating severe aphthous stomatitis.
Oropharyngeal dysphagia and Esophageal Candidiasis
Esophageal thrush is a yeast infection which happens to the throat & mouth.
People with Esophageal with HIV can have hard time eating and swallowing food.
For a HIV patient who has esophageal candidiasis their chief complaint is that they feel like things are sticking, that food is sticking or their pills are sticking, they’re having a hard time swallowing.

As it can be in the picture above Esophageal Candidiasis appears on both throat and tongue of the HIV patient.
Above were the different types of lesions, ulcers, candidiasis appearing on the tongue due to HIV infection. Although, in many cases, once cannot conclude with certainty that the person is HIV positive. The person with symptoms is required to get tested to for HIV in a HIPAA complaint Lab. As a contribution from our end, we can provide you with the HIV testing with coupon code of $10 (discount).
Source
https://www.cdc.gov/hiv/basics/whatishiv.html
Data of the NICBl NIH gov. PMC4344974