Gonorrhea is a major public health concern in the United States more than 800,000 new infections occur each year. As many people don’t have symptoms fewer than half are detected and reported to CDC untreated gonorrhea can cause serious health problems.
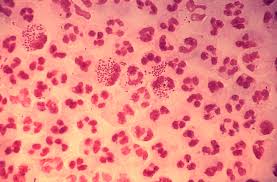
Gonorrhea’s microscopic image
For women, it can increase their risk of a life-threatening ectopic pregnancy.
For men and women, the infection can cause conditions that can lead to infertility.
Also read : Gonorrhea symptoms Prevention in men and women
It can also increase a person’s risk of getting or giving HIV. Medication to treat gonorrhea has been around for decades but the bacteria has grown resistant to nearly every drug ever used to treat it.
History of Gonorrhea treatment and it’s resistance
In the 1980’s, resistance to penicillin and tetracycline grows and they are no longer recommended to treat gonorrhea. Fluoroquinolones are the leading drugs to treat gonorrhea in the 1990s but the bacteria was adapting to the drugs.
By the 2000s resistance to plural quinolones steadily takes hold. CDC modifies treatment recommendations throughout much of the decade to keep pace. In 2000 the drug is no longer recommended to treat people infected in Asia or the Pacific Islands.
In 2002 this recommendation extends to California.
By 2004, CDC no longer recommends it for men who have sex with men in the UnitedStates.
By 2007, resistance is so widespread that CDC no longer recommends, fluoroquinolones to anyone in the U.S.
Also read : Why and how gonorrhea is developing resistance to every antibiotics.
Only one class of antibiotic is successful currently in treating Gonorrhea
To treat gonorrhea only one class of antibiotics known as Cephalosporins is successful. There are two main cephalosporins to treat gonorrhea. 1) The oral drugs cefixime and 2) The injection ceftriaxone.
In 2010 CDC takes additional measures to combat resistance recommending dual treatment with either cefixime or an increased dose of ceftriaxone and azithromycin or doxycycline.
CDC’s updates treatment recommendation for Gonorrhea treatment
But just two years later in 2012, CDC updates treatment recommendations again in response to data suggesting the oral cephalosporin
cefixime is becoming less effective. Gonorrhea is slowly becoming harder and harder to treat today, we are down to one last recommended treatment option.
Only working Gonorrhea treatment
Dual treatment with an injection of Ceftriaxone and an oral dose of Azithromycin. Little now stands between us and untreatable gonorrhea. There are
already troubling signs, with the last recommended treatment. Abroad, infections resistant to ceftriaxone have been detected in several countries and within the US.
There are troubling signs already, resistance to azithromycin has been found in states like Nebraska, Idaho, Illinois, Iowa, Texas, California, Georgia, Alabama and in few parts of West Virginia and Kentucky. There are no reports of treatment failure when used together as of yet. But drug resistance is rising and the pipeline for new drugs is shrinking. Our last treatment option won’t last forever. We must keep drug-resistant gonorrhea as a leading priority.
Prevention is only been a cure, in case of incurable gonorrhea
-
- Practice safer sex: Talk to your partner about sexual history.
- Use Condoms: try not to avoid the use of condoms especially when in a new relationship, if you are not aware of your partner’s sexual health status.
- Avoid sexual contacts in case of any symptoms of possible STD
- Government body for controlling disease should: Increasing the reach of resistance testing, include more and more masses.
- Use the above-tested results to supply correct antibiotics to the patient.
- Find hotspot, predict potential outbreak using available data.
- We need an improved monitoring system to rapidly detect resistance effect.
- Go for routine STD testing once in 6 months even if you don’t have symptoms as some STDs are asymptotic (indicates no symptoms) while some STD can take up to 6 months before they can be detected in the blood.